Racial/ethnic disparities in treatment pattern and time to treatment for adults with glioblastoma in the US
Quinn T. Ostrom, Halle L. Krebs, Nirav Patil, Gino Cioffi, Jill S. Barnholtz-Sloan
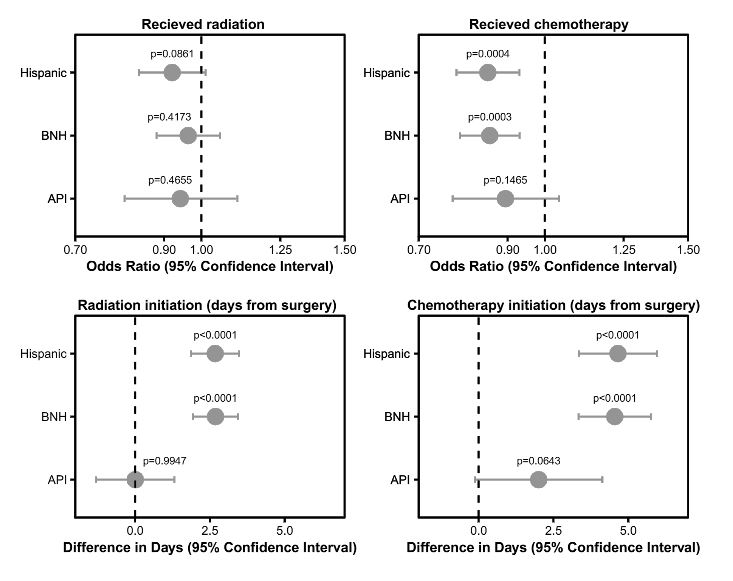
This study examines variation in treatment pattern and time to treatment by race/ethnicity, and the extent to which this affects survival. The authors examined data from the National Cancer Database (NCDB) for adults ≥ 40 with glioblastoma from 2004 to 2016 (N = 68,979). Treatment patterns and time to treatment by race/ethnicity were compared using univariable and multivariable logistic and linear regression models, respectively, and adjusted for known prognostic factors and factors potentially affecting health care access. They found that Black non-Hispanics (BNH) and Hispanics were less likely to receive radiation and less likely to receive chemotherapy as compared to White non-Hispanics (WNH). Time to radiation initiation was approximately two days longer and time to chemotherapy initiation was about four 4 days longer in both groups in comparison to WNH. The authors conclude that both race/ethnicity and treatment timing significantly affected survival time, and this association remained after adjustment for known prognostic factors.
Brain tumors and COVID-19: the patient and caregiver experience
Mathew R Voisin, Kathy Oliver, Stuart Farrimond, Tess Chee, Jean Arzbaecher, Carol Kruchko, Mary Ellen Maher, Chris Tse, Rosemary Cashman, Maureen Daniels, Christine Mungoshi, Sharon Lamb, Anita Granero, Mary Lovely, Jenifer Baker, Sally Payne, Gelareh Zadeh
Since the COVID-19 pandemic began, thousands of medical procedures and appointments have been canceled or delayed. To assess how brain tumor patients and their caregivers are navigating access to care during the pandemic, researchers developed and fielded an online survey that was completed by nearly 2000 people from 33 countries. Results show that as a result of COVID-19, brain tumor patients and caregivers are experiencing significant stress and anxiety.
A comparison of relative survival and cause-specific survival methods to measure net survival in cancer populations.
Makkar N, Ostrom QT, Kruchko C, Barnholtz-Sloan JS
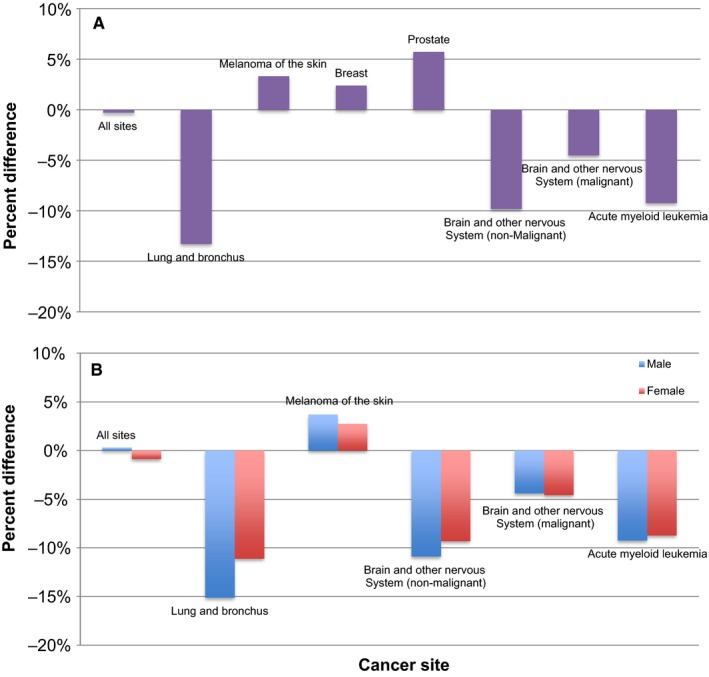
Accurate cancer survival statistics are necessary for describing population-level survival patterns and measuring advancements in cancer care. Net cancer survival is measured using two methods: cause-specific survival (CSS) and relative survival (RS). Both are valid methodologies for estimating net survival and are used widely in medical research. In these analyses, we compare CSS to RS at selected cancer sites.
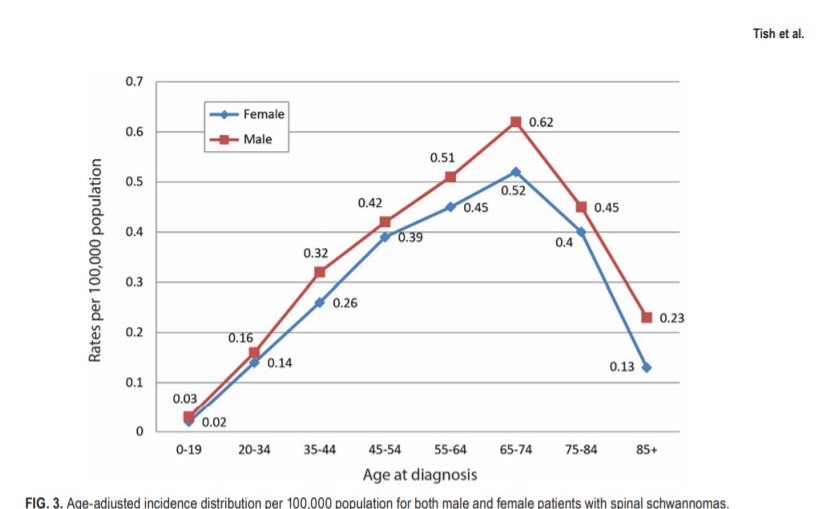
The epidemiology of spinal schwannoma in the United States between 2006 and 2014
Shahed Tish, MD, Ghaith Habboub, MD, Min Lang, MD, MS, Quinn T. Ostrom, PhD, MPH, Carol Kruchko, BS, Jill Barnholtz-Sloan, PhD, Pablo F. Recinos, MD, and Varun R. Kshettry, MD.
Spinal schwannoma remins the third most common interadural spinal tumor following spinal meningioma and ependymoma. The available literature is generally limited to single-institution reports rather than epidemiological investigations. This article describes the epidemiology of spinal schwannoma in the U.S. from January 1, 2006, through December 31, 2014.
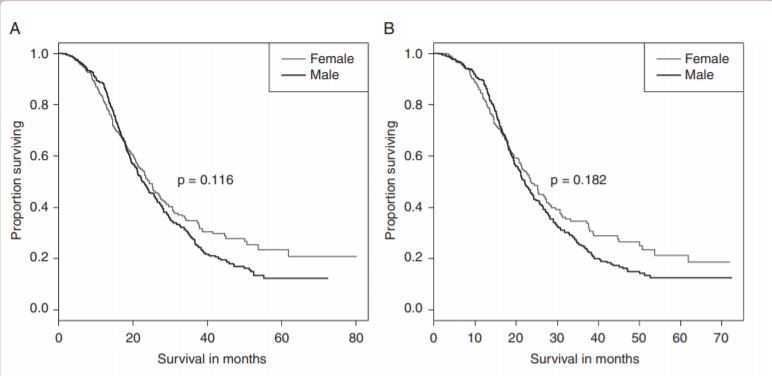
Sex is an important prognostic factor for glioblastoma but not for nonglioblastoma
Haley Gittleman, Quinn T. Ostrom, LC Stetson, Kristin Waite, Tiffany R. Hodges, Christina H. Wright, James Wright, Joshua B. Rubin, Michael E. Berens, Justin Lathia, James R. Connor, Carol Kruchko, Andrew E. Sloan, and Jill S. Barnholtz-Sloan
Glioblastoma (GBM) is the most common and most malignant glioma. Nonglioblastoma (non-GBM) gliomas (WHO Grades II and III) are invasive and also oftern fatal. This study, was done to determine whether sex differences exist in glioma survival. Using the NCDB data, there was statiscially significant female survival advantage in GBM, but not in non-GBM.
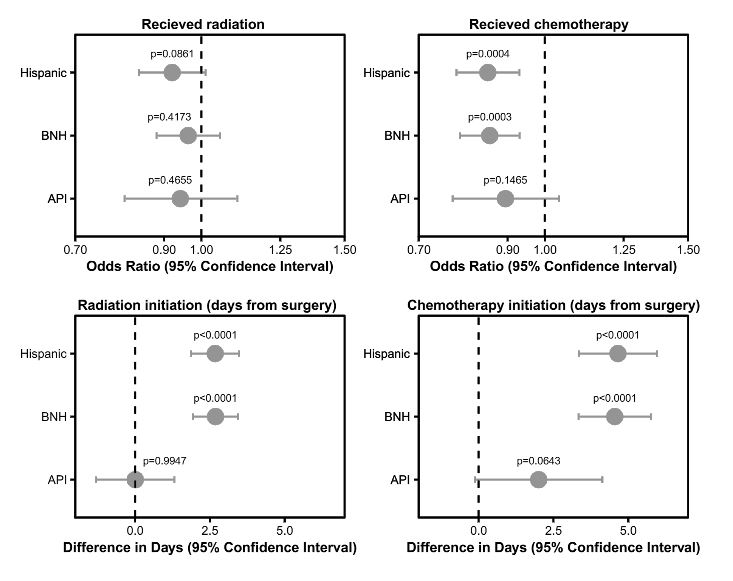
Racial/ethnic disparities in treatment pattern and time to treatment for adults with glioblastoma in the US
Quinn T. Ostrom, Halle L. Krebs, Nirav Patil, Gino Cioffi, Jill S. Barnholtz-Sloan
This study examines variation in treatment pattern and time to treatment by race/ethnicity, and the extent to which this affects survival. The authors examined data from the National Cancer Database (NCDB) for adults ≥ 40 with glioblastoma from 2004 to 2016 (N = 68,979). Treatment patterns and time to treatment by race/ethnicity were compared using univariable and multivariable logistic and linear regression models, respectively, and adjusted for known prognostic factors and factors potentially affecting health care access. They found that Black non-Hispanics (BNH) and Hispanics were less likely to receive radiation and less likely to receive chemotherapy as compared to White non-Hispanics (WNH). Time to radiation initiation was approximately two days longer and time to chemotherapy initiation was about four 4 days longer in both groups in comparison to WNH. The authors conclude that both race/ethnicity and treatment timing significantly affected survival time, and this association remained after adjustment for known prognostic factors.